Authors:
Juan Carlos Díaz, Jorge Marín, Julián Aristizabal, Cesar Niño, Oriana Bastidas, Mauricio Duque
Text:
Cardiac resynchronization therapy (CRT) has established clinical benefits in the management of heart failure with decreased left ventricular ejection fraction (LVEF) and left bundle branch block (LBBB). Since its introduction, the technique has changed little, requiring implantation of a coronary sinus lead (BIVP) effectively achieving CRT. Although this has been associated with a decrease in morbidity (with a reduction in the rate of hospitalization due to failure) and all-cause mortality, BIVP has several drawbacks and almost 1 in 3 patients will not present an adequate clinical response1.
One of the biggest drawbacks of CRT is that ventricular depolarization is transmitted using working myocardium, whose conduction speed is up to 4-6 times lower than that of the cardiac electrical system. In this way, although interventricular dyssynchrony is significantly improved compared to that observed in patients with LBBB, intraventricular synchrony is lower than the native depolarization given by the conduction system. The first attempts to perform conduction system stimulation used His bundle stimulation, and although excellent interventricular and intraventricular synchrony was achieved in some patients, technical difficulties, as well as high battery consumption and high risk of dislocation, did not allow this technique to be widely adopted2-4.
More recently, a novel technique was described to achieve left bundle branch pacing and capture (LBBAP) 5 .Although initially used in patients requiring ventricular pacing without heart failure, the theoretical benefits of this technique for use in CRT have been quickly recognized by several working groups. Compared with BIVP, LBBAP has shown a significant increase in LVEF and reduction in QRS duration (an indirect measure of interventricular synchrony, but which has a prognostic impact in patients with failure)6.More recently, observational studies have shown a significant impact on the composite outcome of hospitalization for heart failure and death from all causes7. In our experience, the use of LBBAP as first-line CRT in patients with heart failure and LBBB has achieved a significant impact on the cardiovascular outcomes8, mainly due to a decrease in hospitalization for heart failure
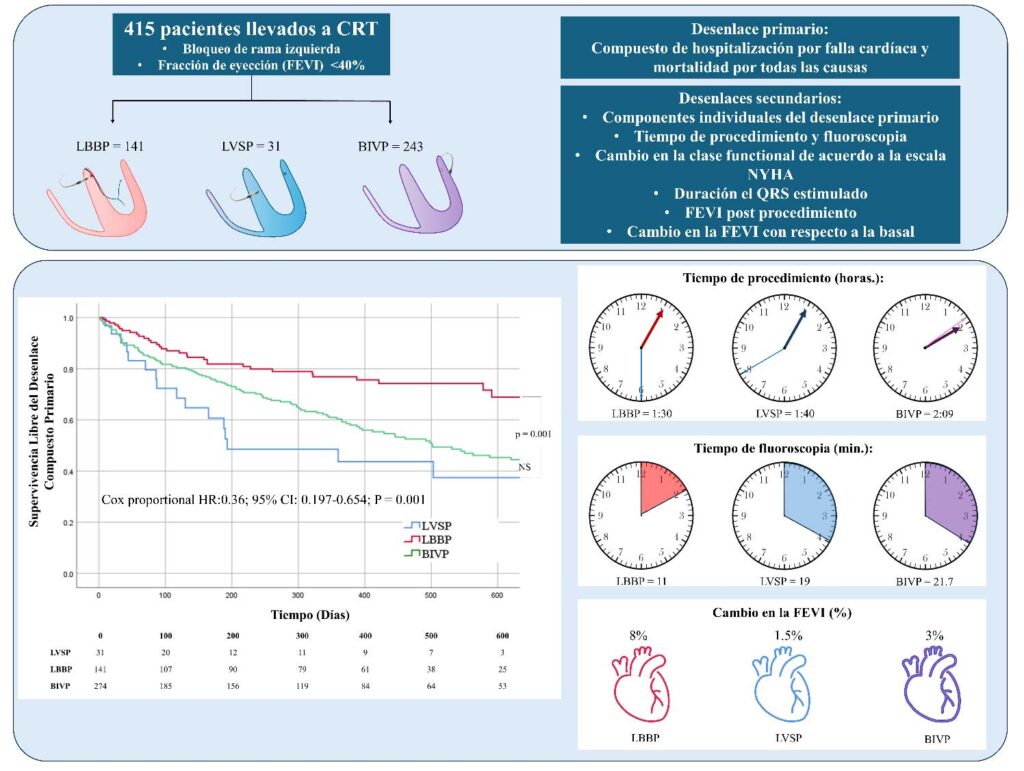
However, there are still questions to be resolved regarding the use of LBBAP in patients with heart failure. Considering that LBBAP refers to both left septal stimulation (LVSP) and left bundle branch stimulation (LBBP), there are questions about whether LVSP and LBBP achieve similar results. It is known that LVSP achieves significant shortening of the QRS and acute hemodynamic improvement, and that these changes are superior to those achieved with other stimulation techniques. 9-10 However, by capturing the conduction system, it would be expected that LBBP would be superior in terms of restoring intraventricular and interventricular synchrony, which would be desirable in patients with heart failure. Recently, we published our experience comparing both stimulation strategies (Central Figure). 11 In total, 415 patients were included (LBBP: n = 141; LVSP: n = 31; BIVP: n = 243; 30.1% women), with a follow-up time of 399 (Q1-Q3: 249.5-554.8) days. Interestingly, LBBP was associated with greater survival free of the primary composite outcome compared with LVSP and BIVP, given mainly by a reduction in the rate of hospitalizations for heart failure without significant differences in the risk of death from all causes. There were no differences in the primary outcome between LVSP and BIVP. Interestingly, achieving capture of the left branch was not associated with a longer procedure or fluoroscopy time. During follow-up, there was a marked improvement in LVEF and functional class in patients taken to LBBP compared with the other two groups, with no significant differences between LVSP and BIVP. These results lead us to think that in patients with heart failure who are going to be taken to CRT with LBBAP, an attempt should be made by all possible means to achieve capture of the left branch. However, even in the worst case, LVSP could be similar in outcomes to BIVP; However, the low number of patients in this group forces us to wait for these results to be confirmed.
Almost simultaneously, a study was published in which the LBBP strategy was compared vs. LVSP. 12 Although the majority of patients in this study had a structurally healthy heart, in patients with structural heart disease the LBBP strategy was associated with longer procedure and fluoroscopy time. There was no difference in LVEF improvement between LBBP and LVSP in this study. What could be the reason for these differences in results compared to ours? In addition to the differences in operators and populations, one of the main differences is that, in our study, every possible means was attempted to achieve LBBP, and LVSP was only accepted when it was not possible to achieve LBBP leading to higher procedure times and fluoroscopy, while in the study by Cano e cols. in a group of patients, LVSP was chosen as the first choice. This would explain the longer time for LVSP in our study. Regarding improvement in LVEF, in some patients in the study by Cano e cols. taken to LVSP, LBBP was achieved, while in patients in whom an LBBP strategy was applied, branch capture was only achieved in 63.5% of patients, which could reduce the differences between the groups.
What is the future of cardiac resynchronization? Today, BIVP continues to be the main strategy for many working groups worldwide. Considering the theoretical benefits, the high success rate of the procedure, in addition to the relatively short learning curve and the results of observational and some randomized studies, we consider that LBBAP is currently a strong contender in CRT. In our group it is used as a first line, and it is possible that this practice will become standard in the coming years, and the adoption of this technique could increase once better tools are available. It is possible that, in the future, the use of leadless devices (such as the Wise TRC®) will allow a more individualized approach, in which a small device is implanted (which favors endothelialization) in the area of the left branch (in patients with left bundle branch block) or in the later activation zone (in patients with indeterminate bundle branch block). Meanwhile, for many of us, LBBAP is the strategy to use to achieve CRT.
Conflicts of interest: Juan Carlos Díaz is a Medtronic speaker and Proctor for left bundle branch stimulation. The other authors declare no conflicts of interest.
References
1. Leclercq C, Burri H, Delnoy PP, Rinaldi CA, Sperzel J, Calò L, Concha JF, Fusco A, Al Samadi F, Lee K, Thibault B. Cardiac resynchronization therapy non-responder to responder conversion rate in the MORE-TRC MPP trial. EuropaceOct 5 2023;25.
2. Upadhyay GA, Vijayaraman P, Nayak HM, Verma N, Dandamudi G, Sharma PS, Saleem M, Mandrola J, Genovese D, Tung R. His Corrective Pacing or Biventricular Pacing for Cardiac Resynchronization in Heart Failure. Journal of the American College of CardiologyJul 9 2019;74:157-159.
3. Lustgarten DL, Crespo EM, Arkhipova-Jenkins I, Lobel R, Winget J, Koehler J, Liberman E, Sheldon T. His-bundle pacing versus biventricular pacing in cardiac resynchronization therapy patients: A crossover design comparison. Heart rhythm : the official journal of the Heart Rhythm SocietyJul 2015;12:1548-1557.
4. Vijayaraman P, Naperkowski A, Subzposh FA, Abdelrahman M, Sharma PS, Oren JW, Dandamudi G, Ellenbogen KA. Permanent His-bundle pacing: Long-term lead performance and clinical outcomes. Heart rhythm : the official journal of the Heart Rhythm SocietyMay 2018;15:696-702.
5. Huang W, Su L, Wu S, Xu L, Xiao F, Zhou X, Ellenbogen KA. A Novel Pacing Strategy With Low and Stable Output: Pacing the Left Bundle Branch Immediately Beyond the Conduction Block. Can J CardiolDec 2017;33:1736.e1731-1736.e1733.
6. Wang Y, Zhu H, Hou X, et al. Randomized Trial of Left Bundle Branch vs Biventricular Pacing for Cardiac Resynchronization Therapy. Journal of the American College of CardiologySep 27 2022;80:1205-1216.
7. Vijayaraman P, Sharma PS, Cano Ó, et al. Comparison of Left Bundle-Branch Area Pacing to Biventricular Pacing in Candidates for Resynchronization Therapy. Journal of the American College of CardiologyMay 10 2023.
8. Diaz JC, Sauer WH, Duque M, et al. Left Bundle Branch Area Pacing Versus Biventricular Pacing as Initial Strategy for Cardiac Resynchronization. JACC Clin ElectrophysiolMay 19 2023.
9. Rijks J, Luermans J, Heckman L, van Stipdonk AMW, Prinzen F, Lumens J, Vernooy K. Physiology of Left Ventricular Septal Pacing and Left Bundle Branch Pacing. Cardiac electrophysiology clinicsJun 2022;14:181-189.
10. Heckman LIB, Luermans J, Curila K, Van Stipdonk AMW, Westra S, Smisek R, Prinzen FW, Vernooy K. Comparing Ventricular Synchrony in Left Bundle Branch and Left Ventricular Septal Pacing in Pacemaker Patients. Journal of clinical medicineFeb 17 2021;10.
11. Diaz JC, Tedrow UB, Duque M, et al. Left Bundle Branch Pacing vs Left Ventricular Septal Pacing vs Biventricular Pacing for Cardiac Resynchronization Therapy. JACC Clin ElectrophysiolDec 1 2023.
12. Cano Ó, Jover P, Ayala HD, Navarrete-Navarro J, Osca J, Izquierdo M, Navarro J, Martínez-Dolz L. Left bundle branch pacing versus left ventricular septal pacing as a primary procedural endpoint during left bundle branch area pacing: Evaluation of two different implant strategies. Journal of cardiovascular electrophysiologyJan 2024;35:120-129.